Understanding Transarterial Chemoembolization (TACE):
Transarterial chemoembolization, commonly referred to as TACE, is a specialized procedure used primarily in the treatment of hepatocellular carcinoma (HCC), the most common type of primary liver cancer.
It is also utilized for treating hepatic lesions that are not amenable to surgical resection or liver transplantation.
The Procedure:
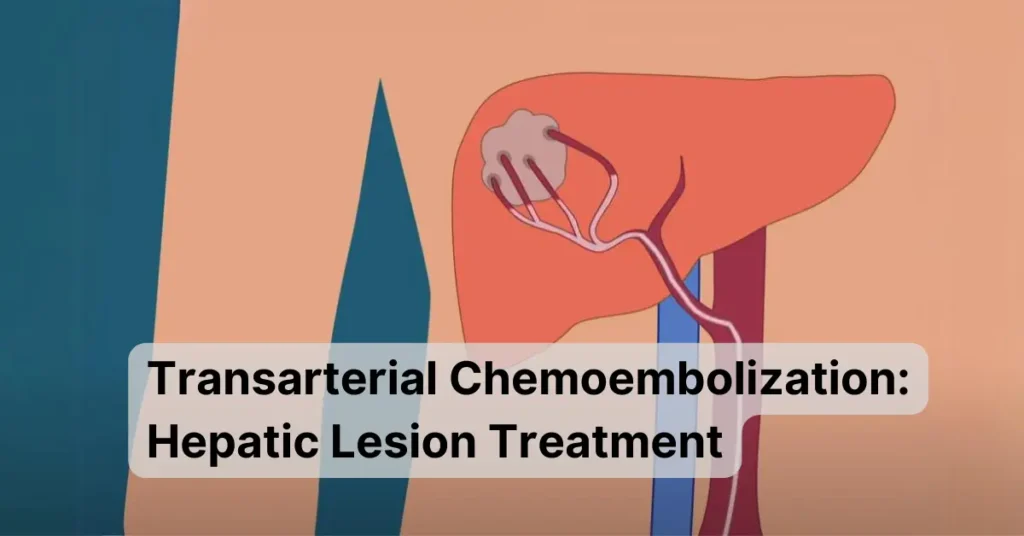
During a TACE procedure, a catheter is inserted into the artery that supplies blood to the liver (the hepatic artery). Through this catheter, chemotherapy drugs, typically mixed with a special oily substance called lipiodol, are directly delivered to the tumor site.
The chemotherapy drugs target cancer cells within the liver while minimizing systemic exposure and side effects.
Following the chemotherapy infusion, the blood supply to the tumor is deliberately obstructed (embolized) using tiny particles or beads. This embolization process cuts off the tumor’s blood supply, effectively starving it of nutrients and oxygen, which leads to tumor shrinkage and destruction.
Benefits of Transarterial Chemoembolization:
- Minimally Invasive: TACE is performed through a small incision, resulting in less trauma to surrounding tissues and quicker recovery compared to traditional surgery.
- Targeted Treatment: By delivering chemotherapy drugs directly to the tumor site, TACE maximizes the therapeutic effect while minimizing systemic side effects.
- Tumor Control: TACE can help control tumor growth, relieve symptoms, and improve overall survival rates in patients with unresectable liver tumors.
- Repeatable Procedure: TACE can be repeated multiple times, offering a viable treatment option for patients with recurrent or residual tumors.
Considerations and Side Effects:
While TACE is generally well-tolerated, it may be associated with certain side effects, including:
- Post-embolization syndrome: This temporary condition may cause fever, abdominal pain, nausea, and fatigue.
- Liver function abnormalities: TACE can lead to transient liver enzyme elevations, which usually resolve on their own.
- Complications: Rarely, TACE may result in more serious complications such as liver abscess, bile duct injury, or liver failure.
Patients need to discuss the potential risks and benefits of TACE with their healthcare provider before undergoing the procedure.
Future Directions and Innovations:
The field of interventional oncology, including TACE, continues to evolve with ongoing research and technological advancements. Emerging techniques such as drug-eluting beads and radioembolization promise to enhance the efficacy and safety of liver cancer treatment.
Conclusion:
Transarterial chemoembolization (TACE) is a valuable tool in the arsenal against liver cancer, providing a targeted and minimally invasive approach to treating hepatic lesions. By understanding the procedure, benefits, considerations, and potential side effects of TACE, patients and healthcare providers can make informed decisions and work together towards better outcomes in the fight against liver cancer.
Commonly Asked Questions about Transarterial Chemoembolization (TACE)
TACE is a minimally invasive procedure used to treat liver tumors by delivering chemotherapy drugs directly to the tumor site and blocking its blood supply.
Candidates for TACE typically have hepatocellular carcinoma (HCC) or other liver tumors that are not amenable to surgical resection or transplantation.
During TACE, a catheter is inserted into the hepatic artery, and chemotherapy drugs mixed with embolic agents are delivered directly to the tumor site.
TACE offers localized treatment, tumor control, and symptom relief with minimal systemic side effects. It is also a repeatable procedure, allowing for multiple treatments if needed.
Patients are typically sedated or given local anesthesia during the procedure, which may last several hours. Post-procedure monitoring is necessary to watch for any complications.
Common side effects include post-embolization syndrome (fever, abdominal pain, nausea), temporary liver enzyme elevations, and rare complications such as liver abscess or bile duct injury.
Recovery time varies but is generally shorter than traditional surgery. Most patients can resume normal activities within a few days to a week after the procedure.
TACE can effectively control tumor growth, improve symptoms, and prolong survival in patients with unresectable liver tumors, especially when used in combination with other therapies.
Depending on the specific case, alternatives to TACE may include surgical resection, liver transplantation, radiofrequency ablation, or systemic chemotherapy.
Coverage for TACE may vary depending on factors such as the patient’s insurance plan, medical necessity, and specific guidelines. It’s important to check with your insurance provider for details on coverage and potential out-of-pocket costs.



One Comment on “Transarterial Chemoembolization: A Guide to Hepatic Lesion Treatment”