Overview
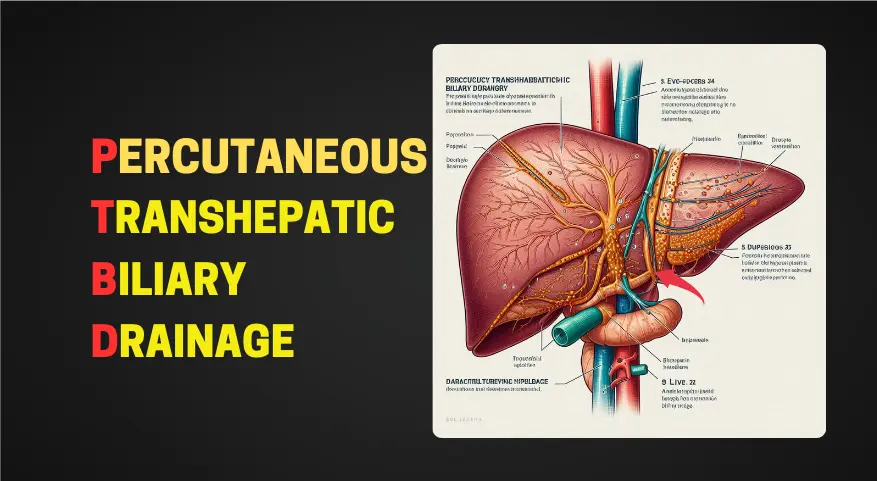
Percutaneous Transhepatic Biliary Drainage (PTBD) is a minimally invasive procedure used to relieve biliary obstruction. It involves the placement of a drainage catheter through the liver to bypass a blockage in the bile ducts. Percutaneous Transhepatic Biliary Drainage is commonly performed when other treatment options, such as endoscopic stenting, are not feasible or effective.
Table of Contents
Indications
Percutaneous Transhepatic Biliary Drainage is indicated for various conditions, including:
- Biliary Obstruction:
- PTBD is primarily used to treat obstructive jaundice caused by conditions such as gallstones, bile duct tumors, or strictures.
- It provides temporary relief by allowing bile to drain directly from the liver into an external drainage bag.
- Preoperative Biliary Decompression:
- In cases where surgery (such as pancreaticoduodenectomy or liver transplantation) is planned, PTBD can be performed to decompress the biliary system before the procedure.
- Reducing jaundice and improving liver function prior to surgery can enhance patient outcomes.
Procedure
- Patient Preparation:
- The patient lies on their back.
- The skin over the right upper abdomen is cleaned and sterilized.
- Local anesthesia is administered to numb the area where the procedure will take place.
- Image Guidance:
- The interventional radiologist or gastroenterologist uses fluoroscopy or ultrasound to guide the procedure.
- A thin needle is inserted through the skin and into the liver.
- The needle is advanced into the bile ducts.
- Contrast dye is injected to visualize the biliary anatomy.
- Catheter Placement:
- A flexible catheter (a thin tube) is threaded over a guidewire.
- The catheter is positioned within the bile ducts.
- It may be placed directly into the liver or through the liver tissue.
- The catheter’s external end is connected to a drainage bag.
- Drainage and decompression:
- The bile flows through the catheter and drains externally.
- This bypasses the obstruction, relieving symptoms such as jaundice and abdominal pain.
- The catheter remains in place to maintain drainage.
- Post-Procedure Care:
- The patient is monitored for any complications.
- PTBD catheters may remain in place for days or weeks, depending on the underlying condition.
Benefits of Percutaneous Transhepatic Biliary Drainage (PTBD)
- Symptomatic Relief:
- PTBD provides rapid relief from symptoms associated with biliary obstruction, such as jaundice, abdominal pain, and itching.
- By allowing bile to drain externally, it reduces the pressure within the bile ducts and liver.
- Preoperative Optimization:
- For patients scheduled for surgery (e.g., pancreaticoduodenectomy or liver transplantation), PTBD can be performed before the procedure.
- Preoperative biliary decompression improves liver function, reduces jaundice, and enhances surgical outcomes.
- Avoidance of Emergency Surgery:
- PTBD can prevent the need for emergency surgery in cases of severe biliary obstruction.
- By relieving the blockage, it stabilizes the patient’s condition and allows for planned, elective procedures.
- Bridge to Definitive Treatment:
- PTBD serves as a temporary solution while awaiting definitive treatment (e.g., surgery, endoscopic stenting, or chemotherapy).
- It buys time for further evaluation and management.
- Minimally Invasive Approach:
- PTBD is performed percutaneously (through the skin) using image guidance.
- It avoids the need for open surgery and reduces recovery time.
- Customizable Drainage:
- The catheter can be adjusted to control the rate of bile drainage.
- This flexibility allows tailoring the drainage to the patient’s specific needs.
- Improved Quality of Life:
- By alleviating symptoms, PTBD enhances the patient’s overall quality of life.
- It restores appetite, reduces discomfort, and improves sleep.
Complications
While Percutaneous Transhepatic Biliary Drainage is generally safe, potential complications include:
- Bleeding:
- Risk: During the PTBD procedure, there is a possibility of bleeding from the liver or surrounding blood vessels.
- Management: Close monitoring during and after the procedure helps detect any bleeding promptly. If significant bleeding occurs, additional interventions may be necessary, such as blood transfusions or embolization to stop the bleeding.
- Infection:
- Risk: Any invasive procedure carries a risk of infection. The insertion site (where the needle or catheter is placed) can become infected.
- Signs: Signs of infection include redness, warmth, swelling, pain, or drainage at the insertion site.
- Prevention: Strict sterile techniques during the procedure minimize the risk. Antibiotics may be given prophylactically.
- Treatment: If an infection occurs, antibiotics are prescribed.
- Catheter Dislodgement:
- Risk: The PTBD catheter may accidentally move or become dislodged.
- Consequences: Dislodgement can lead to inadequate drainage or even complete obstruction.
- Prevention: Proper securing of the catheter and patient education on care are essential.
- Management: If dislodgement occurs, the catheter needs repositioning or replacement.
- Liver Injury:
- Risk: The liver tissue can be damaged during catheter placement or manipulation.
- Consequences: Liver injury may cause bleeding, bile leakage, or infection.
- Prevention: Skilled operators using image guidance minimize this risk.
- Treatment: If liver injury occurs, it may require additional procedures or surgical intervention.
- Other Rare Complications:
- Pneumothorax: Rarely, the lung can be punctured during needle insertion, leading to air accumulation in the chest cavity.
- Bile Leak: Leakage of bile into the abdominal cavity can occur.
- Allergic Reaction: Some patients may have an allergic reaction to contrast dye used during imaging.
Conclusion
Percutaneous Transhepatic Biliary Drainage is a valuable technique for managing biliary obstruction. It provides symptomatic relief and allows for preoperative optimization in select cases. As with any medical procedure, individual patient factors and the underlying condition guide treatment decisions. Consultation with a gastroenterologist or interventional radiologist is essential to determine the most appropriate approach for each patient.
Commonly Asked Questions about Percutaneous Transhepatic Biliary Drainage (PTBD)
- PTBD is a minimally invasive procedure used to relieve biliary obstruction by creating a pathway for bile drainage. It involves inserting a catheter through the skin and liver directly into the bile ducts to allow bile to flow out.
- PTBD is performed in an interventional radiology suite under sterile conditions. It involves inserting a needle through the skin and liver into the bile duct, followed by advancing a guidewire and then placing a drainage catheter over the guidewire.
- PTBD is commonly performed to alleviate biliary obstruction caused by conditions such as bile duct stones, strictures (narrowing), tumors, or post-surgical complications.
- Patients are typically given local anesthesia at the puncture site, which minimizes discomfort during the procedure. However, some patients may experience mild discomfort or pressure during the insertion of the catheter.
- The duration of a PTBD procedure varies depending on factors such as the complexity of the obstruction and the patient’s anatomy. On average, the procedure may take around 30 minutes to an hour.
- While PTBD is generally safe, it carries certain risks, including bleeding, infection, bile leakage, pneumothorax (if the procedure involves the right liver lobe), and catheter dislodgement. These risks are typically low but can occur.
- The duration of catheter placement varies depending on the underlying condition being treated and the patient’s response to treatment. In some cases, the catheter may remain in place temporarily until the obstruction resolves, while in others, it may be left in place long-term for palliative drainage.
- After PTBD, patients may experience improvements in symptoms such as jaundice, abdominal pain, and nausea as bile flow is restored. They will be monitored closely for any signs of complications and may be discharged home with instructions for care and follow-up.
- Patients may be advised to follow a special diet or avoid certain foods temporarily after PTBD, depending on the underlying condition and individual medical needs. It’s essential to follow the instructions provided by healthcare providers for optimal recovery.
- PTBD can be performed on patients with liver disease; however, careful consideration is given to factors such as liver function, coagulation status, and overall health before proceeding with the procedure. The benefits and risks are weighed on a case-by-case basis.